The atherogenic index of plasma (AIP) is a predictor for the severity of coronary artery disease
 Logistic regression analysis-CAD and non-CAD group
Logistic regression analysis-CAD and non-CAD groupAbstract
Objective: Dyslipidemia is a key risk factor for coronary artery disease (CAD). This study aimed to investigate the correlation between the atherogenic index of plasma (AIP) and the severity of CAD.
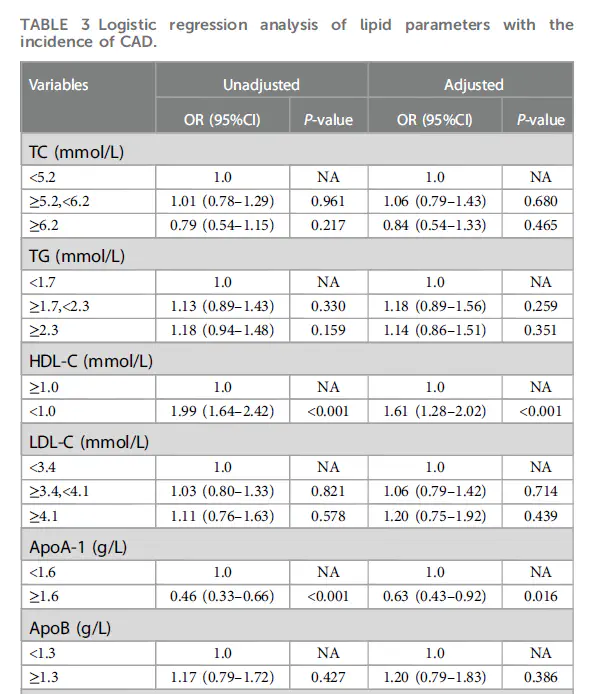
Methods: 2,491 patients were enrolled in this study and analyzed retrospectively, including 665 non-CAD patients as the control group and 1,826 CAD patients. The CAD patients were classified into three subgroups according to tertiles of SYNTAX score (SS). Non-high-density lipoprotein cholesterol (Non-HDL-C) was defined as serum total cholesterol (TC) minus serum high-density lipoprotein cholesterol (Non-HDL-C), atherogenic index (AI) was defined as the ratio of non-HDL-C to HDL-C; AIP was defined as the logarithm of the ratio of the concentration of triglyceride (TG) to HDL-C; lipoprotein combine index (LCI) was defined as the ratio of TC∗TG∗ low-density lipoprotein cholesterol (LDL)to HDL-C; Castelli Risk Index I (CRI I) was defined as the ratio of TC to HDL-C; Castelli Risk Index II (CRI II) was defined as the ratio of LDL-C to HDL-C.
Results: The levels of AIP (P < 0.001), AI (P < 0.001), and LCI (P = 0.013) were higher in the CAD group compared with the non-CAD group. The Spearman correlation analysis showed that AIP (r = 0.075, P < 0.001), AI (r = 0.132, P < 0.001), and LCI (r = 0.072, P = 0.001) were positively correlated with SS. The multivariate logistic regression model showed CRI I (OR: 1.11, 95% CI: 1.03–1.19, P = 0.005), CRI II (OR: 1.26, 95% CI: 1.15–1.39, P < 0.001), AI (OR: 1.28, 95% CI: 1.17–1.40, P < 0.001), AIP (OR: 2.06, 95% CI: 1.38–3.07, P < 0.001), and LCI (OR: 1.01, 95% CI: 1.01–1.02, P < 0.001) were independent predictors of severity of CAD After sadjusting various confounders.
Conclusion: CRI I, CRI II, AIP, AI, and LCI were independent predictors of the severity
of CAD, which could be used as a biomarker for the evaluation of the severity of CAD.