Cohort Study:the optimal timing for non-culprit coronary artery PCI
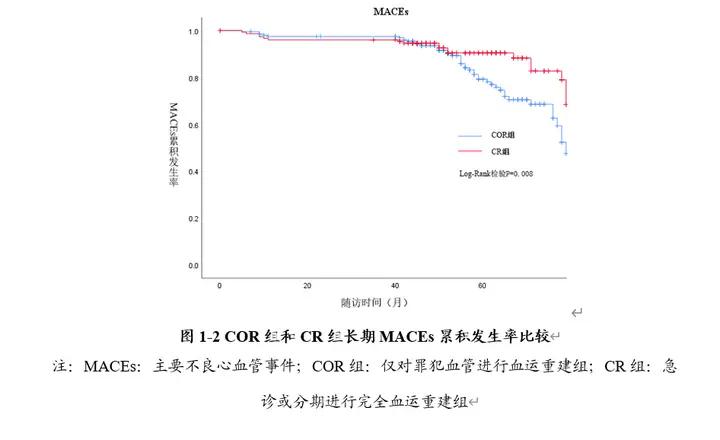 Comparison of Long-term Cumulative Incidence Rates of MACEs between the COR Group (bule line) and the CR Group (red line)
Comparison of Long-term Cumulative Incidence Rates of MACEs between the COR Group (bule line) and the CR Group (red line)I designed the entire retrospective cohort study, conducted follow-up of included patients through telephone and electronic medical records, and ultimately performed comprehensive and detailed data analysis. This included using PASS software for sample size calculation in the initial stages and later utilizing SPSS software for generating Kaplan-Meier Survival Curve and conducting COX regression analysis.
This project also served as my master’s thesis
Objective The aim of this study was to evaluate the short-term and long-term impact of different revascularization strategies on non-culprit coronary artery in patients with acute ST-segment elevation myocardial infarction (STEMI) complicated with coronary multivessel disease (MVD). Ultimately to determine the optimal timing of revascularization of non-culprit vessels.
Methods A total of 980 patients with STEMI who were successfully treated with primary percutaneous coronary intervention (PPCI) in the Department of Cardiovascular, Zhongnan Hospital of Wuhan University between January 1, 2016, and December 31, 2019, were selected, and 364 patients were finally included. According to the revascularization strategy of the non-culprit vessel, the patients were divided into the culprit-only revascularization group (COR), the complete revascularization group (CR), and the emergency complete revascularization group (ECR), staged revascularization during hospitalization (SR-in), staged complete revascularization after discharge (SR-out). All patients underwent clinical data collection and follow-up. The comparisons between COR and CR, CR and SR, SR-in and SR-out were carried out respectively. The Global Registry of Acute Coronary Events (GRACE) score of the patients was calculated and stratified according to the score. GRACE score≥140 was classified as high-risk patients, and <140 was classified as low-to-intermediate risk patients. Subgroup analysis was performed according to GRACE scores. The short-term primary endpoint is major adverse cardiovascular events (MACEs) within 30 days after the PPCI, which is a composite endpoint consisting of cardiac death and recurrent non-fatal myocardial infarction (MI) within 30 days after the PPCI. The short-term secondary endpoints included all-cause death, cardiac death, recurrent non-fatal MI, and heart failure (HF) within 30 days after the PPCI. The long-term primary endpoint is MACEs that occurred between 30 days and the end of follow-up, which is a composite endpoint consisting of cardiac death, recurrent non-fatal MI, and repeat revascularization. The long-term secondary endpoints were all-cause death, cardiac death, recurrent non-fatal MI, repeat revascularization, definite or probable stent thrombosis, HF, and renal insufficiency that occurred between 30 days and the end of follow-up.
Results Among the included patients, there were 205 patients in the COR group, 159 patients in the CR group, 80 patients in the ECR group, 57 patients in the SR-in group, and 22 patients in the SR-out group. The median follow-up time was 57 months (interquartile range (IQR): 47-69 months), and the maximum follow-up time was 83 months. The long-term follow-up results suggested that compared with COR, complete revascularization (ECR or SR) could significantly reduce the incidence of long-term MACEs (11.9% vs. 22.4%; hazard ratio [HR]: 0.453; 95% confidence interval [CI]: 0.253-0.812; P = 0.008), which was mainly due to the significantly lower risk of cardiac death in the CR group (4.6% vs. 13.9%; HR: 0.345; 95% CI: 0.141-0.846; P = 0.020), the incidence of repeat revascularization events in the COR group was slightly higher than that in the CR group, but there was no significant statistical difference (6.6% vs. 9.0%; HR: 0.684; 95% CI: 0.303-1.543; P = 0.360). There was no significant difference in the incidence of recurrent non-fatal MI, all-cause death, stent thrombosis, HF, and renal insufficiency between the two groups. There was no significant difference in the incidence of short-term and long-term MACEs, all-cause death, cardiac death, recurrent non-fatal MI, repeat revascularization, stent thrombosis, HF, and renal insufficiency between ECR group, SR-in group and SR-out group. According to the subgroup analysis stratified by GRACE score, among high-risk patients (GRACE score≥140), the risk of long-term MACEs in CR group was significantly reduced (13.0% vs. 29.9%; HR: 0.437; 95% CI: 0.191-0.995; P = 0.048). Although there was no significant difference in the risk of long-term MACEs between the ECR group and the SR group in the low-to-intermediate risk subgroup, the incidence of MACEs in the SR group showed a downward trend (6.1% vs. 14.6%; HR: 2.480; 95% CI: 0.215-23.555; P = 0.466).
Conclusions In patients with STEMI and MVD, CR can significantly reduce the occurrence of long-term MACEs compared with COR, and this result is mainly driven by a significant reduction in the incidence of cardiac death. Three non-culprit vessel revascularization strategies (ECR, SR-in, or SR-out) showed no significant difference in reducing the incidence of MACEs in patients. In high-risk patients (GRACE score ≥140), CR can significantly reduce the risk of long-term MACEs.